The healthcare community in Massachusetts – defined by its thoughtful, high-quality care to patients across the continuum – is redoubling its effort to be respectful of the wishes of those facing serious illness.
A variety of resources exist to inform caregivers of the current thinking about serious illness care, to allow them to share best practices, and to guide patients and their families during the most trying of times.
We invite you to check back regularly to this page to review updates and to contact us regarding helpful resources we can add to assist the role of Massachusetts caregivers who are providing serious illness care.

A Simple Step: Designating a Healthcare Agent and Completing a Healthcare Proxy (WEBINAR)
Join MHA and Honoring Choices Massachusetts as we outline how you can take the first important step to designate a healthcare agent and complete a healthcare proxy. »Full Article
NQF - ISSUE BRIEF Strategies for Changes - A Collaborative Journey to Transform Advanced Illness Care
Atul Gawande’s Being Mortal and Paul Kalanithi’s When Breath Becomes Air—both New York Times bestsellers authored by physicians—have engaged citizens, clinicians, and caregivers across the United States in thinking about life-threatening illness,
disease, and death—often taboo subjects in our culture. Through personal stories, the authors have inspired the nation to think about mortality, what matters most in life, and why personal preferences are so often neglected in healthcare decisions.
The healthcare system is beginning to undergo a shift from care geared primarily toward medical or clinical needs to care that addresses the needs of the person as a whole. Person-centered care integrates the preferences of the individual and responds to medical as well as functional, social, and emotional needs. Driving this change is a consumer-focused movement along with the recognition that better patient engagement improves healthcare quality and lowers costs.1 This pivot is critical given the increasing number of older Americans facing advanced or serious illness and the growing cultural diversity of the United States population. Advanced illness may result in impairment of daily activities, reduced mental and physical capabilities, frequent medical treatments and visits, and a higher risk of death—all of which can cause an overall decline in health and quality of life.

Massachusetts Coalition for Serious Illness Care
The Massachusetts Coalition for Serious Illness Care is a diverse set of organizations committed to ensuring that healthcare for everyone in the commonwealth reflects their goals, values and preferences.
Click here to view the list of coalition members and commitments.
The Coalition has established six measurable goals to ensure that:
- Everyone in Massachusetts, 18 or older, has designated a healthcare decision-maker (health care proxy);
- Everyone in Massachusetts, 18 or older, has had a conversation (and continues to have conversations) with their proxy to communicate their goals, values and preferences for care at the end of life;
- All Massachusetts clinicians have appropriate training to facilitate high-quality communication with patients on advance care planning and serious illness;
- Everyone in Massachusetts facing a serious illness has had a high-quality, informed goals and values conversation with their care team;
- All Massachusetts healthcare providers have systems in place to elicit and document goals, values and preferences for patients with serious illness;
- All Massachusetts healthcare providers have systems in place to share patient goals, values and preferences across care settings, to ensure they are accessible regardless of place of care.
 Massachusetts Expert Panel on End-of-Life Care
Massachusetts Expert Panel on End-of-Life Care
Under the state’s reform law, Massachusetts formed the Massachusetts Expert Panel on End-of-Life Care that in 2010 produced this comprehensive report: Patient-Centered Care and Human Mortality: The Urgency of Health System Reforms to Ensure Respect for Patient’ Wishes and Accountability for Excellence in Care.
MOLST
Massachusetts Medical Orders for Life-Sustaining Treatment
MOLST is a standardized medical order form for use by clinicians caring for patients with serious advancing illnesses. It relays instructions between health professionals about a patient's care. MOLST is based on an individual's right to accept or refuse medical treatment, including treatments that might extend life. MOLST is very different from a healthcare proxy form, which is a legal document that transmits your wishes after you have lost capacity. A MOLST form, on the other hand, is a medical document signed by both the clinician and the patient, and is effective as soon as it is signed, regardless of a patient’s capacity to make decisions.

A Simple Step: A Call for Long-Term Healthcare Planning
A coalition of leading organizations is coming together to promote proactive care decision-making by calling on patients to designate a healthcare agent.
»Full Article
A Simple Step: Designating a Healthcare Agent and Completing a Healthcare Proxy (WEBINAR)
Join MHA and Honoring Choices Massachusetts as we outline how you can take the first important step to designate a healthcare agent and complete a healthcare proxy.
»Full Article
How Community Members Can Help A Stressed System
As healthcare organizations and caregivers navigate another challenging winter, the Massachusetts Health & Hospital Association is sharing these basic measures that community members can take to help support the system
»Full Article
MHA Releases Comprehensive Report on the Massachusetts Healthcare Workforce
There are an estimated 19,000 full-time job vacancies across Massachusetts hospitals, which has led to the closure of hospital beds and services, steep financial losses for facilities, and access challenges for patients.
»Full Article
National Healthcare Decisions Day 2025
This National Healthcare Decisions Day, MHA and our coalition members encourage you to take the simple steps necessary to take charge of your healthcare. The coalition is highlighting three key steps for community members: Choose someone you trust to be your designated healthcare agent and have a simple conversation about what’s important to you. Complete a health care proxy form ...» Full Article
Massachusetts e-MOLST Web Portal
New VIDEO. Introduction to MA e-MOLST Web Portal for Honoring Choices Partners. Share with your clinicians and care teams. Tools & Resources to Use the Portal Start Proactive Planning Conversations & Document Care Choices The MA e-MOLST Web Portal offers health care providers and seriously ill, high-risk, and frail adults an effective communication approach to engage in proactive ...» Full Article
9th Annual April National Healthcare Decisions Month
MHA is proud to recognize National Healthcare Decisions Month, in partnership with Honoring Choices of Massachusetts. We recognize the importance of advance care planning and the ability of patients to understand their care options. MHA and our members encourage everyone to take the simple but important steps this month to prepare for the future. Every year the Honoring Choices Partners & ...» Full Article
Being Prepared in the Time of COVID-19
With generous support from the Cambia Health Foundation, Ariadne Labs and The Conversation Project have developed a patient-facing guide on Being Prepared in the Time of COVID-19. This tool can help people take action and be prepared for the pandemic. Read more... ...» Full Article
MA Coalition for Serious Illness Care – Good Talk Campaign
Based on the Coalition’s public messaging research, we have developed the Good Talk Toolkit to be a resource that supplements your organization’s capacity to build awareness and understanding for advance care planning. The messaging and campaign included here are intended to shift the frame of advance care planning away from end of life and life-sustaining treatment choices towards goals of c...» Full Article
WHITE PAPER: “Conversation Ready”: A Framework for Improving End-of-Life Care (2nd Edition)
The resilience of the human body and spirit, the science of modern health care, and the efforts of health care professionals have resulted in a larger number of patients living with increasingly complex illnesses for longer periods of time. As the number of seriously ill patients has risen, so too has the scrutiny of end-of-life care. Stories about poor end-of-life care have become unfortunately ...» Full Article
What is Palliative Care?”
Webinar Recording (Time: 5 minutes) - For Everyone: Learn why Palliative Care is an added layer of support for individuals with serious illness- at any age, any serious illness, and any phase of health. ...» Full Article
For Consumers: “Palliative Care: Aligning the Team Around the Patient”
Webinar Recording (Time: 30 minutes) - For Consumers, Patients, Families and Caregivers can explore Palliative Care and learn key questions to start a discussion with your care providers. Elizabeth J.Collins, MD, Palliative Care Medical Director, Lahey Hospital & Medical Center, provides a framework of the 5 stages of serious illness and how palliative care can be effective at each stage and...» Full Article
For Care Providers: “Palliative Care: Aligning the Team Around the Patient”
Webinar Recording (Time: 30 minutes - Followed by Q & A) -Every care provider can be a "first responder" to help patients diagnosed with a serious illness start a palliative care conversation. Learn key questions to open meaningful discussions with patients & clients. Elizabeth J.Collins, MD, Palliative Care Medical Director, Lahey Hospital & Medical Center, provides a framework of t...» Full Article
Palliative Care for Consumers – Fact Sheet
Palliative Care is specialized health care for individuals diagnosed with a serious illness to manage the pain, symptoms and stress of living with a serious illness. A Palliative Care clinician or a team of care providers, offer an “extra layer of support” in addition to your regular medical care. They can provide emotional and spiritual support for you and your family. Palliative care impr...» Full Article
Honoring Choices “Everyone, Everyday” Initiative
Make a plan for quality care today & everyday. The "Everyone, Everyday" initiative reaches out to all adults to make a personal health care plan within their own language, culture and ability, and receive the best possible care today and everyday, starting at 18 years old and continuing all through their lifetime. Make Your Plan. Then, Help Move it Forward! You can start to make your own p...» Full Article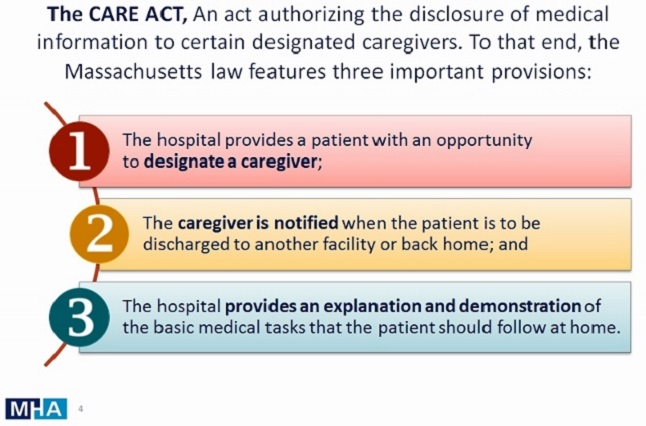
MHA’s CARE Act Guidance – Updated Materials
The Caregiver Advise, Record & Enable (CARE) Act (Chapter 332 of the Acts of 2016), effective November 8, is intended to allow patients over the age of 18, who have been admitted as an inpatient at an acute care hospital, to designate a caregiver and give permission for the hospital to provide medical information to that caregiver. Materials, Fact Sheet and FAQs can be found here... &nbs...» Full ArticleTranslate »