Leading a Culture of Safety: A Blueprint for Success was developed to bridge a gap in knowledge and resources by providing chief executive officers and other health care leaders with a useful tool for assessing and advancing their organization’s culture of safety. This guide can be used to help determine the current state of an organization’s journey, inform dialogue with the board and leadership team, and help leaders set priorities.
Author: admin
MHA’s Guidelines for Healthcare Safety and Violence Prevention (2025 Update)
In response to the increased risk of violence in healthcare settings, the Massachusetts Health & Hospital Association’s Healthcare Safety and Violence Prevention Workgroup (HSVPW) developed guidance to help healthcare facilities use evidence-based practices to create effective healthcare violence prevention programs.
Six years after the initial guidance was released, MHA consulted with the workgroup to produce an updated version: Guidelines for Healthcare Safety & Violence Prevention. The updated guidance provides additional strategies that have emerged over the past few years to support member organizations with maintaining a safety culture, reducing risk of violence, and improving wellbeing and outcomes for patients, visitors, providers, and staff.
This update offers newly revised strategies for a comprehensive approach to healthcare safety and violence prevention across healthcare facilities, including emergency departments, inpatient settings, outpatient clinics, mobile health services, and home healthcare. It also recognizes that because every healthcare organization has its own unique needs, structures, economics, patient populations, and workforce environments, each entity’s response to workplace violence will be different. There is no one single way to implement a workplace violence strategy for a healthcare setting, but these collected strategies can assist.
Over the last few years, the HSVP’s accomplishments include adopting and reporting on a standardized data collection tool, creating a united set of principles for patient-visitor codes of conduct, providing regular education opportunities to disseminate safety and violence prevention strategies from local and national leaders, and advocating for federal and statewide policy changes related to healthcare worker protections. Taken together, these efforts have helped make Massachusetts a recognized national leader in healthcare safety and violence prevention and prompted collaboration and publications with colleagues across the country.
AHA Issue Brief: Building a Safe Workplace and Community — Violence Mitigation in a Culture of Safety
The American Hospital Association’s Hospitals Against Violence (HAV) initiative hosted the American Society for Health Care Risk Management (ASHRM) for a facilitated dialogue to explore challenges and current strategies to mitigate the risk of violence. The discussion fostered an exchange of ideas and solutions that informed this issue brief and accompanying case studies.
From AHA:

In 2021, HAV developed the Building a Safe Workplace and Community framework to guide health care leaders in their efforts to prevent and mitigate violence.
This issue brief, the third of four in the series, examines how hospitals’ violence mitigation efforts can fit effectively into an organization’s culture of safety strategy. The brief includes thought-provoking questions to facilitate discussion of how violence mitigation can be integrated seamlessly into the larger framework of patient and worker safety initiatives, supporting an overall culture of safety. It also explores strategies that leaders could take to best support a culture that mitigates violence as part of larger enterprise efforts.
AHA Issue Brief: Building a Safe Workplace and Community — Providing Trauma Support to Your Workforce Following an Incident or Threat of Violence
The American Hospital Association’s Hospitals Against Violence (HAV) initiative hosted the American Society for Health Care Risk Management (ASHRM) for a facilitated dialogue to explore challenges and current strategies to mitigate the risk of violence. The discussion fostered an exchange of ideas and solutions that informed this issue brief and accompanying case studies.
From AHA:
In 2021, HAV developed the Building a Safe Workplace and Community framework to guide health care leaders in their efforts to prevent and mitigate violence.
This issue brief examines trauma support for hospital and health system team members. It was developed from discussions the HAV Advisory Group had with the Medical University of South Carolina’s National Mass Violence Victimization Resource Center (NMVVRC) team about the challenges and opportunities to provide trauma support to health care workers following an incident or threat of violence.
AHA Building a Safe Workplace and Community: A Framework for Hospital and Health System Leadership
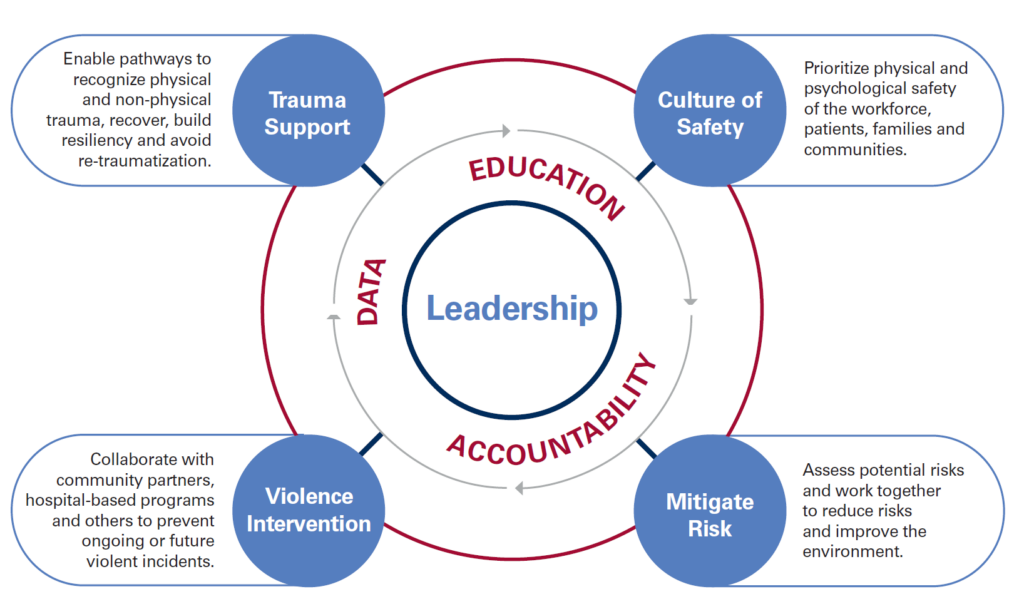
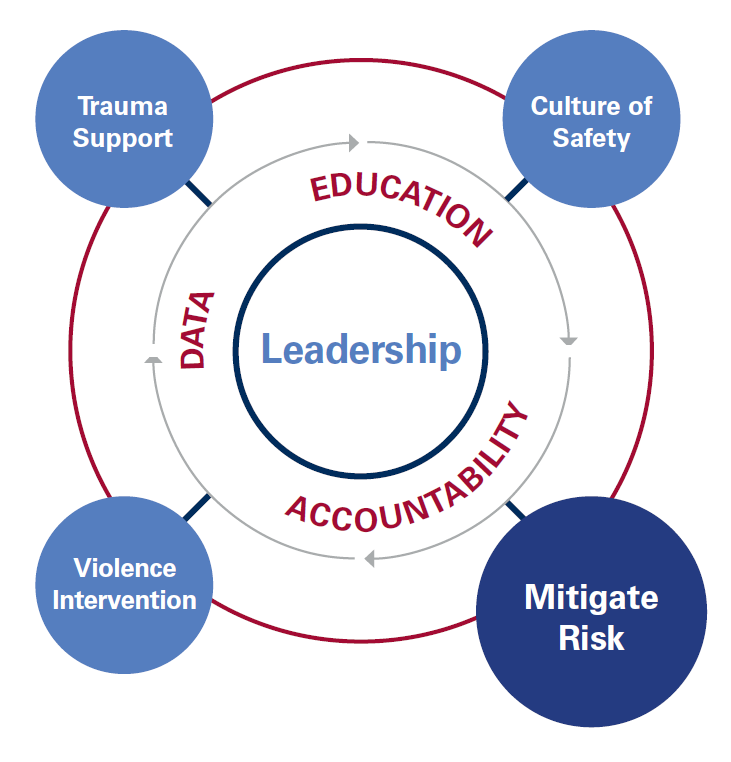
The American Hospital Association’s Hospitals Against Violence (HAV) initiative hosted the American SAHA’s Hospitals Against Violence framework helps guide hospital and health system leadership address the issues of violence in their workplaces, with an emphasis on educating and protecting the workforce. In this effort, we must acknowledge that community violence encroaches into the health care setting, and our workforce is part of the community.
Leadership should push for greater data collection, collective accountability, and ongoing education and training. With this approach, we can achieve the four pillars necessary for implementing a comprehensive violence mitigation strategy: trauma support, violence intervention, culture of safety and mitigating risk.
To learn more about the AHA’s Hospitals Against Violence
initiative, visit www.aha.org/HAV.
AHA Issue Brief: Building a Safe Workplace and Community — Mitigating Risk of Violence
The American Hospital Association’s Hospitals Against Violence (HAV) initiative hosted the American Society for Health Care Risk Management (ASHRM) for a facilitated dialogue to explore challenges and current strategies to mitigate the risk of violence. The discussion fostered an exchange of ideas and solutions that informed this issue brief and accompanying case studies.
From AHA:
In 2021, HAV developed the Building a Safe Workplace and Community framework to guide health care leaders in their efforts to prevent and mitigate violence.
This issue brief examines risk mitigation and marks the first in a series that expand on each domain of the framework: culture of safety, violence intervention, trauma support and risk mitigation. This issue brief is an outgrowth of a series of discussions between hospital and risk management leaders. The brief shares considerations when assessing potential risks, strategies to mitigating violence and insights on making the care environment safer.
American Society for Healthcare Risk Management, Workplace Violence Toolkit
Violence in the workplace continues to be an area that risk managers need to be proactively preparing their institutions to prevent. At the same time, the risk manager needs to know what to do in the event they are faced with an immediate situation. This tool kit is designed to assist in both of these areas.
The Joint Commission, Improving Patient & Worker Safety: Opportunities for Synergy, Collaboration, & Innovation
This monograph is intended to stimulate greater awareness of the potential synergies between patient and worker health and safety activities. Using actual case studies, it describes a range of topic areas and settings in which opportunities exist to improve patient safety and worker health and safety activities.
OSHA, Safety and Health Management Systems: A Road Map for Hospitals
A safety and health management system is a tool to help turn this situation around: a proven, flexible approach to proactively and continually address workplace safety and health issues.1 It provides the overarching framework for planning, implementing, evaluating, and improving all workplace safety and health management efforts.
OSHA, Safe Patient Handling Programs: Effectiveness & Cost Savings
The Safe Patient Handling Programs: Effectiveness and Cost Savings document gives administrators a business case for investing in safe patient handling programs, policies, and equipment, based on real-life findings from hospitals across the United States that have successfully implemented these programs.