 Catheter Associated Urinary Tract Infections (CAUTIs) are an often preventable healthcare- associated infection (HAI) common in hospitals across the country. These infections can be a serious complication for patients, can increase the time they are hospitalized and add to the cost of care. On occasion, antibiotic treatment of CAUTIs can also pose potential health risks for the patient.
Catheter Associated Urinary Tract Infections (CAUTIs) are an often preventable healthcare- associated infection (HAI) common in hospitals across the country. These infections can be a serious complication for patients, can increase the time they are hospitalized and add to the cost of care. On occasion, antibiotic treatment of CAUTIs can also pose potential health risks for the patient.
PLAN: Identifying Issues and Goals
Using a Plan-Do-Study-Act performance improvement model, Milton Hospital launched a comprehensive patient safety initiative program to reduce this type of infection. A multidisciplinary care team consisting of nurses, physicians, clinical educators and Infection Prevention Specialists set a goal to achieve zero incidences of CAUTI for inpatients by October 2010.
After an extensive review of current literature and best practices, Milton Hospital decided to adopt a practice bundle described by the Institute for Healthcare Improvement (IHI). This set of care practices called for more restrictive catheter use, prompt removal, and hygiene management of catheters while inserted and patient and staff education.
DO: Implementing and Reinforcing New Practices
Following this practice bundle as a guide, the hospital updated its catheter insertion criteria to reduce unnecessary catheter use.
"Limiting catheter use and minimizing the duration of its insertion are important strategies to reduce CAUTIs," said Alex Campbell, MSN, RN, EN, BC, Director, Healthcare Quality.
To determine the need for catheter insertion, Milton Hospital purchased a portable bladder ultrasound scanner, which can identify whether the patient is unable to empty his/her bladder fully. This device often eliminates the need for urinary catheterization in some patients. Nursing staff was trained in the proper use of this device. Additionally, all nursing staff were re-educated on the proper sterile procedure for inserting catheters, as well as the appropriate post-insertion management process.
Procedures were developed and implemented to improve communication between nurses and physicians regarding catheterized patients. On a daily basis, all catheterized patients are evaluated to determine the earliest opportunity to remove the catheter. Also on a daily basis, clinical educators monitor staff for compliance with updated insertion and management procedures. Educational materials, including brochures and posters, were developed not only to reinforce staff training, but also to inform patients of their role in reducing the risk of infection related to catheter use.
STUDY: Measuring the Affects of Process Changes
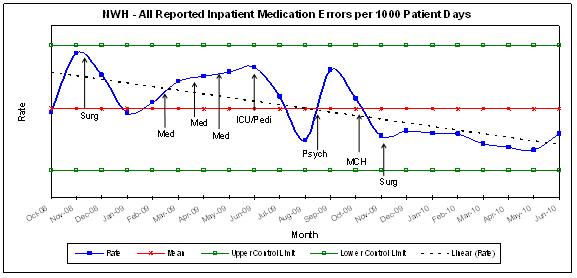
To establish a reliable means of tracking CAUTI rates, the hospital developed data collection processes relating to this infection type and relating to compliance with new practice expectations. Data is reviewed on an ongoing basis by Infection Prevention, Nursing, Medical Staff and hospital leadership.
In August 2009 (prior to the roll out of the practice bundle), Milton Hospital experienced four incidents of healthcare-associated CAUTIs in that month. After introducing its performance improvement plan in September 2009, a significant reduction in the incidence of CAUTIs was achieved. Between September 2009 and March 2010 (seven months) only three incidents of CAUTI occurred at Milton Hospital. This is an 89% reduction in comparison to August 2009.
In addition, the Urinary Catheter Device Utilization rate, which measures the percentage of patients who had a catheter in place and the duration of catheter use, dropped from 25.9% in September 2009 to 18.1% by March 2010 (a decrease of more than 30%). As a final measure of success, in October 2009, the Centers for Medicare and Medicaid (CMS), based on best practice recommendations, required hospitals to ensure that all post-operative patients with urinary catheters had them removed when appropriate by their second post-operative day. Although this is a new expectation for hospitals, by January 2010 Milton Hospital achieved and has maintained a compliance score of 100% with this expectation.
ACT: Maintaining and Improving Momentum
Today, Milton Hospital continues to work toward its goal of eliminating CAUTIs. Ongoing analysis and investigation identify new opportunities for improvement, as the Plan-Do-Study-Act process continues to evolve.
Healthcare Acquired Infections
Healthcare acquired infections (HAIs), also known as nosocomial infections, are infections that patients get while receiving treatment for medical or surgical conditions. HAIs occur in all settings of care, including hospitals, surgical centers, ambulatory clinics, and long-term care facilities such as nursing homes and rehabilitation facilities.