Through the work of over 35 national, leading organizations, the Dementia Friendly America initiative is catalyzing a movement to more effectively support and serve those across America who are living with dementia and their family and friend care partners. The lead organizations represent all sectors of community and are collectively leveraging their national reach to activate their local affiliates, members and branches to convene, participate in and support dementia friendly community efforts at a local level.
Author: admin
Dementia Friendly Massachusetts Initiative
An estimated 5.4 million people in the United States and more than 120,000 Massachusetts residents are living with dementia, which is a general term for changes in thinking such as memory loss and difficulty planning and communicating. Dementia may be caused by Alzheimer’s disease or other conditions. Despite the widespread impact of dementia, lack of information, fear, and stigma can prevent those affected from feeling safe, socially connected, and able to thrive in their communities.
CDC’s Get Ahead of Sepsis Campaign
The Centers for Disease Control and Prevention launched Get Ahead of Sepsis, an educational initiative to protect Americans from the devastating effects of sepsis. This initiative emphasizes the importance of early recognition and timely treatment of sepsis, as well as the importance of preventing infections that could lead to sepsis.
Sepsis is the body’s extreme response to an infection. It is life-threatening, and without timely treatment, sepsis can rapidly lead to tissue damage, organ failure, and death. Each year in the U.S., more than 1.5 million people develop sepsis, and at least 250,000 Americans die as a result.
Public education is critical to save lives since, for many patients, sepsis develops from an infection that begins outside the hospital.
Get Ahead of Sepsis calls on healthcare professionals to educate patients, prevent infections, suspect and identify sepsis early, and start sepsis treatment fast. In addition, this work urges patients and their families to prevent infections, be alert to the symptoms of sepsis, and seek immediate medical care if sepsis is suspected or for an infection that is not improving or is getting worse.
“Detecting sepsis early and starting immediate treatment is often the difference between life and death. It starts with preventing the infections that lead to sepsis,” said CDC Director Brenda Fitzgerald, M.D. “We created Get Ahead of Sepsisto give people the resources they need to help stop this medical emergency in its tracks.”
Get Ahead of Sepsis offers exciting new resources for healthcare professionals and patients – including fact sheets, brochures, infographics, digital and social media, and shareable videos for both the healthcare professional and for the consumer.
NCOA – Falls Prevention Conversation Guide

Why is falls prevention important?
FALLS ARE COMMON
Falls are the leading cause of fatal and non-fatal injuries for older Americans.
1 in 4 older adults falls each year.
Every 11 seconds, an older adult is treated in the emergency room for a fall.
Every 19 minutes, an older adult dies from a fall.
FALLS CAN CAUSE SERIOUS INJURIES
Falls result in injuries, such as hip fractures, broken bones, and head injuries. In fact, more than 2.8 million older adults are treated in emergency departments annually because of a fall, resulting in over 800,000 hospitalizations.
FALLS ARE COSTLY
The average hospital cost for a fall injury is over $30,000. Falls, with or without injury, carry a heavy burden on quality of life.
After a fall, many older adults develop a fear of falling and, as a result, limit their activities and social engagements.
Fear of falling can result in further physical decline, depression, social isolation, and feelings of helplessness.
FALLS IMPACT CAREGIVERS, TOO
Research has shown that after a care recipient’s first fall, caregivers report a significant increase in caregiver burden, fear of falling, and depression.
Seasonal Influenza A (H3N2) Activity & Antiviral Treatment of Patients with Influenza
In the United States (U.S.), influenza activity has increased significantly over recent weeks with influenza A(H3N2) viruses predominating so far this season. In the past, A(H3N2) virus-predominant influenza seasons have been associated with more hospitalizations and deaths in persons aged 65 years and older and young children compared to other age groups. In addition, influenza vaccine effectiveness (VE) in general has been lower against A(H3N2) viruses than against influenza A(H1N1)pdm09 or influenza B viruses. Last season, VE against circulating influenza A(H3N2) viruses was estimated to be 32% in the U.S.
CDC expects that VE could be similar this season, should the same A(H3N2) viruses continue to predominate. For this reason, in addition to influenza vaccination for prevention of influenza, the use of antiviral medications for treatment of influenza becomes even more important than usual. The neuraminidase inhibitor (NAI) antiviral medications are most effective in treating influenza and reducing complications when treatment is started early. Evidence from previous influenza seasons suggests that NAI antivirals are underutilized in outpatients and hospitalized patients with influenza who are recommended for treatment.
Resources:
CDC guidance about antiviral treatment and prophylaxis for influenza can be found here.
CDC guidance about flu diagnosis can be found here.
The recently redesigned MDPH Flu website has information for providers and the general public. Click on ‘Information for Healthcare and Public Health Professionals’ for such provider resources as influenza control guidance, model standing orders, screening forms and planning clinics and campaigns.
Click here for the CDC Health Advisory on Seasonal Influenza A(H3N2) Activity and Antiviral Treatment of Patients with Influenza
ED Visits After Inpatient Discharge in MA – Recording 11-15-17 Webinar
In July 2017, Center for Health Information and Analysis (CHIA) released this report on ED visits after inpatient discharge. The analysis provided a broad look at the patients who return to the ED, whether or not they are readmitted to the inpatient level of care. These “revisits” to the ED may represent an opportunity to prevent a hospital readmission or may be avoidable.
Following the release of the report, MHA, CHIA and Collaborative Healthcare Strategies organized a webinar to share the key findings from the report and discuss how it can be used to inform and improve care transition to reduce avoidable acute-level hospital use.
On November 15, 2017 MHA, CHIA, & Collaborative Healthcare Strategies offered a webinar on emergency department (ED) visits within 30 days of an inpatient discharge in Massachusetts.
MHA is now offering a recording of the webinar available here. The webinar runs for approximately one hour. The slides from the webinar, without the recorded narrative, are here.
American Hospital Association’s Hospital Against Violence Campaign
The AHA 's Hospitals Against Violence Hope (#HAVhope) Friday is a digital media campaign focused on bringing national attention to ending all forms of violence and encouraging hospitals, health systems and community organizations to stand together against violence. Become a supporter by tweeting or submitting a photo that highlights your efforts of combatting violence in the community you serve.
Eugene WoodsThe June 9 HAVhope Day of Awareness is an outgrowth of a Hospital Against Violence campaign initiated by the AHA Board of Trustees to give voice to hospital efforts that combat violence in their communities and their facilities. While violence is different from one community to another, it has become a major public health and safety issue for nearly everyone in our country. In fact, according to the Centers for Disease Control and Prevention (CDC), more than 2.3 million people are treated in U.S. emergency departments each year for violent injuries and violence costs more than $85 billion annually in medical expenses and lost productivity. What is constant, however, is the commitment of hospitals and health systems in helping their employees, patients and communities address violence in whatever form it may take.
Quick Facts:
More than 55,000 deaths and 2.5 million violence-related injuries occur every year (AHA)
On average, nearly 20 people per minute are physically abused by an intimate partner in the United States (NCADV)
12 percent of nonprofit hospitals identified community violence prevention as a priority need in their community health needs assessment (AHA)
Podcasts on Violence Prevention
As part of the Hospitals Against Violence campaign, the AHA interviewed various hospitals across the country that have institutionalized a violence prevention program upon learning violence is a prominent health issue in the communities they serve. Listen to some initiatives hospitals have adopted to combat violence in their community.
Honoring Choices “Everyone, Everyday” Initiative
Make a plan for quality care today & everyday. The “Everyone, Everyday” initiative reaches out to all adults to make a personal health care plan within their own language, culture and ability, and receive the best possible care today and everyday, starting at 18 years old and continuing all through their lifetime.
Make Your Plan. Then, Help Move it Forward! You can start to make your own personal health care plan and put it into action with your care providers using the free Honoring Choices Getting Started Tool Kit. Then, inform and empower your family members, friends, neighbors and all adults in your community — anywhere adults live, work and gather. It’s easy to do. We’ll provide the free tools and programs.
Everyone can help: community groups, faith and cultural groups, and local business can get involved. Your support can help us reach all Massachusetts adults to open the door to health care planning and improve quality care for all.
BMC Links Patients to Outpatient Addiction Treatment Services
Caregivers at Boston Medical Center (BMC) have released a study outlining how the hospital’s Addiction Consult Service (ACS) may be making a significant dent in the problem of inpatients with substance use disorder (SUD) relapsing into addiction – and being readmitted – shortly after discharge.
Numerous studies have shown that many inpatients (15% by one Massachusetts study) have an active SUD, and that they’re likely to be readmitted within 30 days of discharge. But treating a patient for substance use disorder in addition to whatever other forms of treatment the hospital is providing often does not occur.
“Barriers to inpatient initiation of medications for [opioid use disorder] include the limited availability of outpatient providers and programs, lack of insurance coverage, and federal privacy regulations that make coordinating and integrating medical and addiction care difficult,” BMC researchers wrote in the Journal of Substance Use Treatment.
To address the problem, BMC created its Addiction Consult Service in July 2015. The physician-RN ACS team meets with the patient, provides brief bedside counseling, initiates addiction-treatment medications, and formulates discharge planning.
“Discharge work for the ACS included collaborating with the primary hospital medical team, social work, and hospital case management, as well as coordination with and linkage to post-discharge addiction providers,” according to the study. “The ACS regularly collaborated with social work within the hospital and held weekly joint rounds with the Psychiatry Consult and Liaison service.”
Two BMC outpatient clinics and three local methadone clinics were the main post-discharge linkages.
BMC reports that over the first 26 weeks, the ASC received 367 referrals resulting in 337 consults. (Some patients left against medical advice, refused to be seen, etc.)
“Like heart disease can cause a heart attack or a stroke, addiction causes many acute injuries requiring immediate attention, but we can’t simply treat that issue without delving deeper to address the root cause,” said Alex Walley, MD, MSc, a general internist at BMC’s Grayken Center for Addiction who also oversees the addiction medicine fellowship. “Our goal is to engage willing patients in treatment and work with them on a plan that will keep them healthy and safe now and in the future.”
MHA’s V.P. of Clinical Affairs Pat Noga, RN, FAAN, who is involved in the association’s work on opioids, said BMC’s ACS work is well-known within the caregiving community and provides a template for work by other hospitals or state efforts going forward.
Click on the link to read the full study: Addiction consultation services – Linking hospitalized patients to outpatient addiction treatment.
And click here to read about the efforts of MHA’s Substance Use Disorder Prevention and Treatment Task Force that has developed guidelines for hospital to use in addressing the opioid crisis.
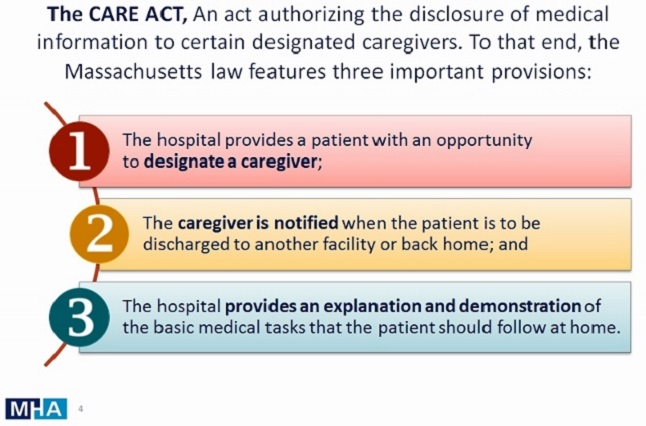
MHA’s CARE Act Guidance – Updated Materials
The Caregiver Advise, Record & Enable (CARE) Act (Chapter 332 of the Acts of 2016), effective November 8, is intended to allow patients over the age of 18, who have been admitted as an inpatient at an acute care hospital, to designate a caregiver and give permission for the hospital to provide medical information to that caregiver.
Materials, Fact Sheet and FAQs can be found here…