According to the Institute of Medicine (IOM), "medication-related error … is one of the most common types of error, substantial numbers of individuals are affected, and it accounts for a sizable increase in health care costs."* In order to decrease the potential for medication-related errors, Newton-Wellesley Hospital launched a major patient safety initiative in 2009 - the implementation of an electronic Medication Administration Process (eMAP).
The eMAP process maximizes the use of clinical information systems to standardize the encoding of data used to identify medications, patients, and clinicians and to protect patients from preventable medication errors. In addition, electronic documentation allows readily available viewing access by all healthcare providers to the medication administration record. eMAP combines the technology of an electronic Medication Administration Record (eMAR) and bar-code technology to confirm patient, medication, and provider bedside medication verification (BMV). The use of the technology is an additional tool for clinicians to provide safer patient care.
Newton-Wellesley Hospital implemented eMAP across 14 units in 2009. eMAP maximizes the use of clinical information systems and bar-coding to ensure that the right patient receives the correct medication and dose; it also provides warnings to the nurses who administer the medications if there are discrepancies. This initiative required extensive planning from many departments, including clinical informatics, nursing, education, pharmacy, information services, and physicians. More than 120 order sets, 2,000 formulary medications, dose instructions, and administration criteria were evaluated. New hardware required in-depth evaluation and testing. Intensive training and support were provided before, during, and after implementation.
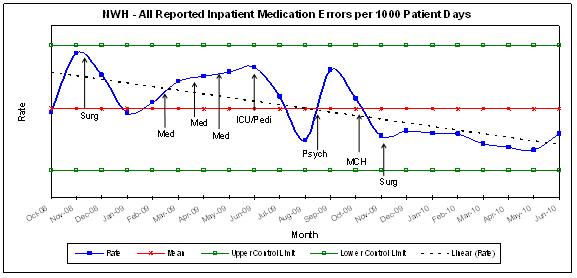
As a way of evaluating the effectiveness of eMAP implementation, the number of medication errors reported in the Safety Reporting System (SRS) was analyzed. The majority of medication errors reported in the SRS are near misses and/or errors that caused no patient harm. Nevertheless they provide an opportunity to review practices and recommend positive changes. An analysis of the data revealed that since implementation of eMAP in November 2008, the rate of reported errors has decreased. Looking at specific points in time (November 2008 & June 2010), the percentage of change for all reported transcription, administration, and total medication errors decreased by 56%, 53%, and 56% respectively.
Additional monitoring is performed quarterly on eMAP quality monitoring day to identify other opportunities to improve the overall performance related to safe medication practices. On these days, staff members observe their peers as they use the process, and data is collected from current medical records. A review of this data allows the team to determine other enhancements in the system, the process, or both. For example, it was recently noted that one oral medication was not being scanned consistently by nursing. Based on further information, it was identified that the medication was packaged in such a way as to make it difficult to scan with the bar-coding technology. Pharmacy has identified a vendor with a more readable bar code and is working with nursing to change the inventory.
This hospital-wide endeavor highlights one step on the journey to continuously improve the quality and safety of the care given to our patients and the efforts and support of all involved in this pursuit.
* Institute of Medicine, To Error is Human; Building a Safer Health System (Washington, DC,: National Academy Press, 2000), p. 28
-- by Sandy Abboud, RN, MPH; Manager, Clinical Informatics
and Sue Scott, RN, Ed.M, Nursing Quality Program Manager

